Osteoporosis of the Spine
As we get older, our bones become more porous and our bone strength decreases. Osteoporosis is a disease in which bones become very weak and more likely to break. It often develops unnoticed over many years, with no symptoms or discomfort until a bone breaks.
Fractures caused by osteoporosis most often occur in the spine. These spinal fractures are called vertebral compression fractures. They are almost twice as common as other fractures typically linked to osteoporosis, such as broken hips and wrists.
Not all vertebral compression fractures are due to osteoporosis. But when the disease is involved, a vertebral compression fracture is often a patient’s first sign of a weakened skeleton from osteoporosis.
Cause
As osteoporosis progresses, the vertebrae weaken and narrow, which can make the patient shorter and cause a severely rounded upper back (“dowager’s hump”).
When the small bones of the spine (vertebrae) weaken from osteoporosis, they can narrow or shrink. This can lead to a rounded back, a hump or a “bent forward” look to the spine. Many people with osteoporosis also note that they are getting shorter over time.
The weakened vertebrae are at a high risk for fracture. A vertebral compression fracture occurs when too much pressure is placed on a weakened vertebra and the front of it cracks and loses height. Vertebral compression fractures are sometimes the result of a fall, although people with osteoporosis can suffer a fracture even when doing everyday things, such as reaching, twisting, coughing, and sneezing
Symptoms
A vertebral compression fracture has a wedged-shaped appearance. The front of the vertebra has cracked and shortened while the back remains intact.
A vertebral compression fracture causes back pain. The pain typically occurs near the break itself. Vertebral compression fractures most commonly occur near the waistline, as well as slightly above it (mid-chest) or below it (lower back).
The pain often gets worse with standing or sitting for a period of time, and is often relieved by rest or lying down. Although the pain may move to other areas of the body (for example, into the abdomen or down the legs), this is uncommon.
Diagnosis
Your appointment will begin with a discussion with your doctor about your symptoms and medical history.
While you are standing, your doctor will examine the alignment, or straightness, of your spine and your posture. your doctor will also push on certain places on your back to try and identify whether your pain is from an injury to the muscle or bones.
To make sure there is no injury to the spinal nerve roots, your doctor will conduct a neurologic examination. This includes testing your reflexes and muscle strength.
X-rays
If your doctor suspects a vertebral compression fracture, he or she will order diagnostic tests to confirm your condition.
Other problems in the spine may also show up on x-rays. Elderly patients with a vertebral compression fracture may also have narrowing of disk space (degenerative disk disease) and/or scoliosis, which is a sideways curve of the spine.
MRI
This test will show any damage to the soft tissues around the fracture (nerves and disks) in better detail. Because of how it shows bone, it may help your doctor determine how old the fracture is.
Bone Scan
A bone scan can pick up a wide range of problems in bone, including fractures. It can also show how old a fracture is.
Computed tomography (CT) scan. This study also shows soft tissue, as well as bone, and can help your doctor evaluate whether the vertebral compression fracture has extended into the spinal canal, where the spinal cord and nerve roots are located.
Bone Density Testing
When you have a vertebral compression fracture, it is important to assess whether you also have osteoporosis, and, if so, how severe the condition is. X-rays will often show thinning of the bone throughout the spine — a condition known as osteopenia. It is a forerunner to osteoporosis, in which the bone becomes much more fragile.
The extent of bone loss can be determined with a bone mineral density scan (DEXA). The results of the DEXA help your doctor estimate your risk for additional fractures in the spine and in other parts of your body. The DEXA results provide important information to help your doctor treat any bone density loss with me
Treatment
Nonsurgical Treatment
Most people who suffer a vertebral compression fracture get better within 6 to 8 weeks without specific treatment to repair the fracture. Simple measures, such as a short period of rest and limited use of pain medications, are often all that is prescribed. In some cases, patients are instructed to wear a brace to restrict movement and allow the vertebral compression fracture to heal.
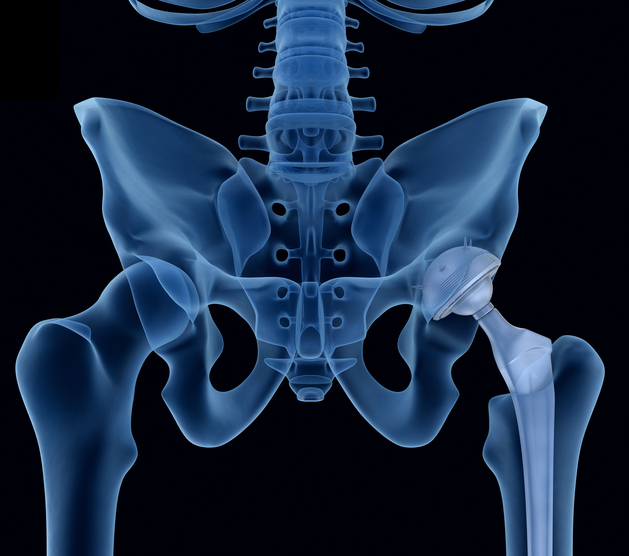
If your doctor has also diagnosed osteoporosis, you are at an increased risk for additional vertebral compression fractures and other fractures, such as to the hip and wrist. your doctor will address treatments for bone density loss during this time.
Surgical Treatment
If you have severe pain that does not respond to initial treatment measures, then surgery may be considered.
In the past, the only surgical options available to patients with a vertebral compression fracture involved extensive procedures. Today, vertebral augmentation procedures offer a minimally invasive alternative.
The two types of vertebral augmentation methods available are kyphoplasty and vertebroplasty. The best candidates for these procedures are patients who suffer severe pain from recent vertebral compression fractures. If you are a candidate for vertebroplasty or kyphoplasty, your doctor will discuss which one may be better for you based on the type of vertebral compression fracture you have.
Kyphoplasty
In a kyphoplasty, a small device called a balloon tamp is inserted into the fractured vertebra. The balloon tamp is inflated from within the vertebra, which restores the height and shape of the vertebral body. When the balloon tamp is removed, it leaves a cavity that is filled with a special bone cement that strengthens the vertebra.
Kyphoplasty can be performed using general anesthesia (which puts you to sleep) or with a local anesthesia (which numbs your body around the fracture). In this procedure, the patient lies face down on the operating table and the surgeon accesses the spine from the back.
After surgery, patients can go back to all their normal activities of daily living as soon as possible, with no restrictions.
These x-rays show (left) a side-view and (right) a front-view of the spine after kyphoplasty surgery.
Vertebroplasty
Vertebroplasty is a technique similar to kyphoplasty, but a balloon tamp is not used to create a space for the cement. Instead, the cement is injected directly into the narrowed vertebra. Like kyphoplasty, this procedure is performed while the patient is lying face down so that the surgeon can access the fractured vertebra from the back.
After this surgery, patients are encouraged to return to their normal, day-to-day activities as soon as possible.
- These x-rays show the needle for a cement injection being inserted into the vertebra during vertebroplasty surgery.